What do you do in case you go to your native pharmacy to fill your month-to-month insulin or different diabetes treatment prescription, solely to seek out that your well being insurer has switched your treatment with out your physician (otherwise you!) figuring out?
This apply is named ‘non-medical switching’ and occurs when a well being insurer removes a lined prescription out of your well being plan or strikes it to the next tier in your plan, making your co-payment prohibitively costly. Plans will normally do that to economize.
The consequences of non-medical switching can fluctuate from a slight annoyance to extraordinarily adverse medical penalties.
On this put up, I’ll clarify why insurance coverage corporations generally swap your diabetes treatment and the choices you’ve for interesting the choice.
How do medical insurance corporations determine which medicine to cowl?
In keeping with Specific Scripts, medical insurance corporations first take a look at the efficacy of a drug, not essentially the price of a drug, when deciding what to cowl.
Well being plans normally have committees made up of physicians and pharmacists who assessment the knowledge that federal regulators used to approve a drug, along with what number of different, comparable medicine are available on the market, earlier than making a ultimate determination.
All well being plans in the USA cowl insulin, it simply will depend on what type they’re keen to cowl.
What’s non-medical switching?
Non-medical switching is a standard cost-saving tactic utilized by many medical insurance plans in the USA.
It occurs when an insurance coverage firm adjustments the phrases of a contract or the price of a medicine for a secure affected person; the “swap” isn’t resulting from medical causes however is commonly a less expensive model that the well being insurer has deemed interchangeable with the previous treatment that the affected person was prescribed.
This apply differs from “step remedy” the place a affected person should “fail” on a drug first earlier than the well being plan will cowl a costlier one.
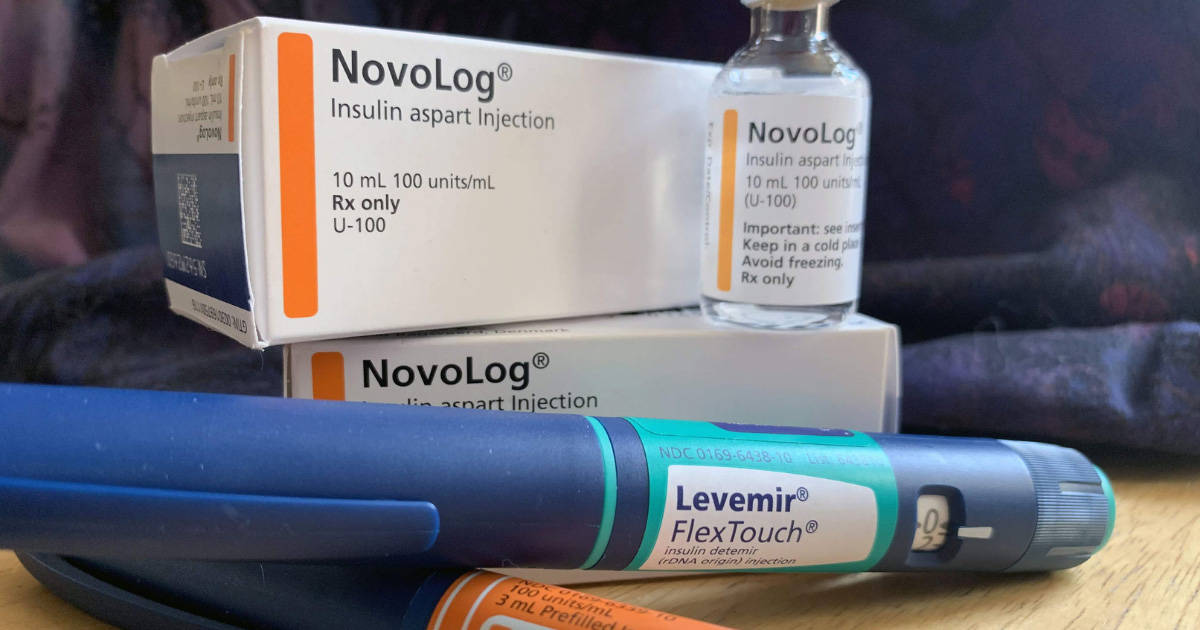
Assume: forcing a affected person with diabetes to make use of an older, human insulin (like R or NPH), and to ultimately have a excessive A1c, earlier than the well being plan will cowl a more recent, sooner, analog insulin, like Humalog or Novolog.
In keeping with the U.S. Ache Basis, non-medical switching prices the USA over $100 billion yearly, and it immediately hurts sufferers who’re in any other case secure on their prescription drugs.
Is non-medical switching at all times an issue?
It’s necessary to notice that non-medical switching just isn’t at all times a nasty factor.
First, the apply just isn’t quite common, so in case you’re newly identified, don’t fear about this till it really turns into an issue.
Second, in case you’re taking a medicine, however your well being plan switches you to a more recent model of the identical drug that works even higher, or a drug that works fully interchangeably along with your previous treatment and also you discover no distinction, then there’s no downside and there’s no cause to fret.
Non-medical switching is a matter in case your well being plan adjustments your treatment to a different treatment that you simply’re unable to take as a result of your well being will endure in case you do.
The way to undo non-medical switching
Having your treatment modified final minute, particularly in case you’re doing effectively on it, might be extraordinarily irritating. The excellent news is that you simply don’t have to just accept these adjustments outright.
There are a number of issues you are able to do to attraction a choice to change your diabetes treatment. Here’s a step-by-step information:
Name your physician
The attraction course of can take time, so instantly notifying your diabetes staff of the adjustments you’ve skilled on the pharmacy counter is important. Your physician can supply recommendation on learn how to change your dosing quantities, if relevant.
In the event you’re unwilling or unable to make use of the newly prescribed treatment, however your previous treatment is now exceedingly costly, the American Diabetes Affiliation and Past Type 1 have gathered a wealth of assets for sufferers who need assistance affording their drugs.
Request your previous treatment
In the event you’ve been on a selected kind of insulin or treatment for a number of years or extra (on the identical medical insurance plan), insurers sometimes received’t change your protection, however it does occur.
In the event you’re unwilling to strive the brand new drug, you must instantly name your medical insurance plan and request your previous treatment.
The well being plan could say that they want a previous authorization (PAR) out of your physician stating that the particular prescription drug they’re requesting is a medical necessity to you, and can’t be used interchangeably with one other, cheaper drug.
A previous authorization request should be submitted by means of your medical skilled – you can not submit one by yourself behalf.
Some individuals run into these points a number of occasions a yr, for a number of drugs, because the PAR course of is a manner for insurers to chop prices (and keep away from overlaying costlier medicine for his or her purchasers).
Have your physician request “99 months” on the prior authorization, so this headache doesn’t grow to be an annual occasion.
In a 2018 examine within the Journal of Present Medical Analysis and Opinion, researchers surveyed 451 individuals with kind 2 diabetes about their experiences with non-medical switching.
After their drugs had been switched, one in 5 had been instructed by their physician that their blood glucose ranges had been considerably or a lot worse than that they had been on their earlier treatment.
About 20% additionally needed to test their blood sugars extra usually than earlier than they switched, which might grow to be a bodily, emotional, and monetary burden.
Moreover, practically 1 in 4 mentioned the non-medical swap negatively impacted their psychological well being.
Request a “peer-to-peer” assessment
In case your well being plan denies your request to your previous treatment again, you’ll be able to request a peer-to-peer analysis, through which your physician confers with a physician from the well being plan to debate why your particular treatment is medically mandatory.
This could generally resolve the issue with out going by means of a prolonged appeals course of.
File an attraction (an inside assessment)
In the event you’re battling the brand new treatment and you can not afford your previous treatment (by paying the upper co-payments or paying out of pocket), your physician can attraction your insurance coverage firm’s determination by requesting an inside assessment.
Remember the fact that it is a prolonged course of and there’s no assure of success. Listed below are the steps in submitting an insurance coverage attraction:
- Collect the denial letter from the earlier makes an attempt to get your previous treatment again. That is generally referred to as a dedication letter.
- Evaluate your Clarification of Advantages doc, to verify the denial wasn’t made in error. You may at all times name your insurer’s customer support line to get extra details about the unique denial.
- Name your physician’s workplace to allow them to know you’re requesting an attraction. They can assist you with writing an attraction letter in your behalf, and even enable you to fill out the proper varieties.
- Hold observe of your blood glucose information for a number of weeks. Sure, we’re bringing out the old-school logbook (or a diabetes app). This can be utilized as proof in your attraction that the brand new drug is inflicting adverse penalties to your diabetes management.
Chris Plourde, who lives with kind 1 diabetes and has skilled non-medical switching, says, “paperwork to substantiate your declare that the brand new treatment isn’t a superb match is vital. In the event you can present documentation that the unique drug labored, normally insurance coverage corporations will likely be okay with it,” she says.
“However you want numerous documentation proving that you simply want it. In the event you get switched, write down your blood glucose readings, write down how the brand new treatment makes you are feeling, write down all of the adjustments you discover.”
File an exterior assessment
Typically inside evaluations don’t work out for the affected person, and the insurance coverage firm sticks with its authentic determination. Don’t fear; you’ll be able to request further inside evaluations, and even request an exterior assessment.
Conducting an exterior assessment signifies that you’ll herald an unbiased third occasion who will determine the matter. Your well being plan’s ultimate denial letter will embrace info on learn how to file for an exterior assessment and the timeframe inside which you need to accomplish that (normally 60 days from the ultimate denial).
After a 3rd occasion has decided in an exterior assessment, the medical insurance plan is legally sure to just accept it.
What are individuals doing about this?
Fortunately, many affected person advocacy organizations are fascinated by fixing this downside to forestall it from taking place to extra individuals. The Hold my Rx marketing campaign is gathering grassroots assist to unfold consciousness about this apply.
Moreover, many states are beginning to ban non-medical switching or restrict the apply.
In the previous couple of years, California and Nevada have adopted such legal guidelines. States like Florida and Tennessee have additionally thought of comparable laws, and Massachusetts has fashioned a fee to analyze the concept. Colorado has banned the apply for some medicine.
Nevertheless you select to get entangled, your well being and diabetes administration ought to by no means be compromised for a well being plan’s backside greenback.